online learning with Doc note master|| Himanshu paneru
UNVEILING THE WORLD OF MEDICALLY IMPORTANT BACTERIA: A COMPREHENSIVE OVERVIEW
Bacteria are prokaryotic organisms, meaning they lack a true nucleus and membrane-bound organelles
SYSTEMIC BACTERIOLOGY
Himanshu Paneru
4/16/20247 मिनट पढ़ें
BACTERIA
· Bacteria are single-celled microorganisms
· Bacteria are prokaryotic organisms, meaning they lack a true nucleus and membrane-bound organelles
· They are among the most abundant and diverse organisms on Earth
· Found in various environments, including soil, water, air, and the bodies of plants & animals.
· They lack a true nucleus and membrane-bound organelles
· They play vital roles in various ecosystems and have a significant impact on human health
CHARACTERISTICS
· Some major characteristics of bacteria are:
1. Prokaryotic Cells:
Bacteria are prokaryotes, which means they lack a nucleus and other membrane-bound organelles found in eukaryotic cells.
Their genetic material, a single circular DNA molecule.
Genetic material located in the cytoplasm in an area called the nucleoid.
2. Unicellular Organisms:
Bacteria exist as single-celled organisms.
Each bacterial cell is capable of carrying out all the functions necessary for its survival, reproduction, and metabolism independently.
3. Cell Wall:
Bacteria have a cell wall that surrounds the cell membrane.
The cell wall provides structural support and protection against changes in the external environment.
Composition of the cell wall varies different in every bacterial species.
On the basis of cell wall bacteria are classified as –
Ø Gram-positive or
Ø Gram-negative.
4. Diverse Shapes:
Bacteria exhibit a wide range of shapes, including –
Ø Spherical shape (cocci)
Ø Rod-shaped (bacilli)
Ø comma (vibrios)
Ø Spiral-shaped (spirilla or spirochetes).
Some bacteria may also have complex shapes or forms such as filamentous or branching structures.
5. Flagella and Pili:
Flagella are whip-like structures that allow bacteria to move in liquids, while pili are thin, hair-like appendages that aid in adherence to surfaces.
6. Metabolic Diversity:
They can be categorized as –
Ø Autotrophs: capable of synthesizing their own organic compounds from inorganic sources.
Ø Heterotrophs: obtain organic compounds from external sources.
7. Reproduction:
Bacteria reproduce asexually through a process called binary fission.
BINARY FISSION: bacterial cell divides into two identical daughter cells, allowing for rapid population growth.
Some bacteria can also exchange genetic material through processes like conjugation, transformation, and transduction, contributing to genetic diversity and adaptation.
8. Ubiquity and Abundance:
Bacteria are ubiquitous and can be found in almost every environment on Earth, including soil, water, air, and the bodies of plants and animals.
They are among the most abundant and diverse organisms on the planet.
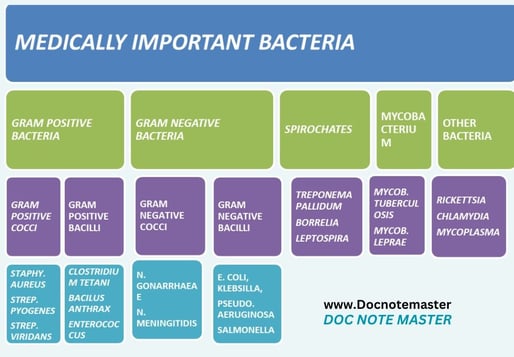
MEDICALLY IMPORTANT BACTERIA
GRAM POSITIVE BACTERIA
A. GRAM POSITIVE COCCIAM POSITIVE COCCI .RAM POSITIVE COCCI GRAM POSITIVE COCCI .
STAPHYLOCOCUS AUREUS
# Morphology:
· Gram-positive bacteria.
· It appears in clusters resembling grapes when viewed under a microscope.
· Size: 1 µm in diameter.
· Motility: They are Non-motile
· Non-spore-forming
· Capsulated: Non-capsulated.
· Facultative Anaerobic
# Pathogenesis:
· Staphyl. Aureus is an important pyogenic organism.
· Thick creamy pus is formed in staphyl. Infection.
Ø Source of infection – Contaminated food, patient with septic lesion, infected blood or body fluid, etc.
Ø Mode of transmission – Staphy. aureus are most often transmitted by direct or indirect content, inhalation, ingestion & inhalation.
Ø Route of transmission – respiratory tract, GI tract, etc.
Ø Incubation period – about 2-6 hours in food born staphylococcus aureus.
· Disease may be classified as
Cutaneous infection: It Include postules, boils, abcesses, burn & wound.
Deep infection: It Include Osteomyelitis, tonsilitis, pharyngitis, sinusitis, meningitis.
Food poisoning: It may follow 2-6 hours after ingestion contaminated food.
Nosocomial infection: It refers hospital acquired disease.
Skin exoflative disease: commonly seen in children. Example – staphylococcus scalded skin syndrome (SSSS).
Toxic shock syndrome: women’s are commonly affect.
# Lab diagnosis:
Ø Specimen:
Common samples include pus, wound swabs, sputum, blood, urine, or other body fluids.
Ø Microscopy:
After gram stain Gram-positive cocci in clusters seen.
Ø Culture:
Grow on culture media such as nutrient agar, macconkry agar, blood agar, milk agar & mannitol salt agar.
Incubate at 37*C for overnight.=
Ø Biochemical reaction:
Coagulase test – positive
Phosphatase test – positive
Catalase test – positive
Oxidase test – negative
Ø Antibiotic susceptibility testing:
Susceptibility is determined by various method such as disk-diffusion.
STREPTOCOCCUS PYOGENES
# Morphology
· Gram-positive bacteria
· Shape: spherical or oval
· Size: About 0.5 to 1.0 µm in diameter.
· Arrangement: Arrange in chain.
· Capsule: Some strains of possess capsule.
· Motility: Non-motile
· Spore: Non-sporing
# Pathogenesis
Streptococcus pyogenes produce pyogenic infection that spread locally along with lymphatic & blood stream.
Ø Source of infection – Contaminated food, lesion, infected blood or body fluid such as saliva, wound, or nasal secretions, etc.
Ø Mode of transmission – transmitted by direct or indirect content, ingestion & inhalation.
Ø Route of transmission – respiratory tract, GI tract, etc.
Ø Incubation period – about 3 to days.
A. SUPPRATIVE INFECTION:
1) RESPIRATORY INFECTION –
Sore throat (acute tonsillitis and/or pharyngitis) is the most common streptococcal diseases.
Tonsillitis is more common in older children and adults.
2) Skin & soft tissue infection –
Strep. Pyogenes causes subcutaneous infection of skin lymphangitis & cellulitis.
It include wound & burn.
It may lead to fetal septicemia.
Strep. Pyogenes is also known as ‘FLASH EATING BACTERIA’.
Bacterial infection such as Erysipelas & impetigo.
3) Streptococcal toxic shock syndrome –
TSS is a condition in which the entire organ system is collapse, leading to death.
4) Genital infection –
Aerobic & Anerobic streptococci are normal inhabitant of female genital tract.
Important causative agent of puerperal sepsis.
5) Other supprative infection
Strep. Pyogenes may cause abscess in internal organ such as brain, lungs, liver & kidney.
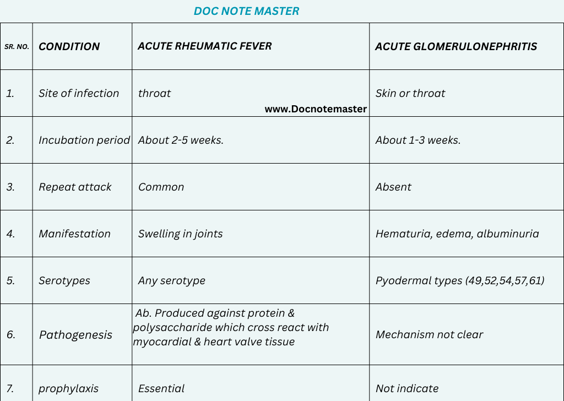
B. NON-SUPPRATIVE INFECTION:
# Lab diagnosis
Ø Specimen:
Throat swab
Wound swab
Pus
CSF
Blood
Ø collection & transport:
Specimen should be collected on sterile container.
Pike’s medium is used for transport
Ø Microscopy:
Gram staining - Gram positive bacteria seen in chain formation.
Ø Culture:
Best grow in blood agar at 37®C for 24-48 hours in presence of 5 – 10% CO2.
Ø Colony morphology:
Colony of strep. Pyogenes are-
Shape – round
Size- 0.5-1mm
Surface – smooth
Color – grey
Opacity – translucent
Ø Biochemical reaction:
Camp test – negative
Catalase – negative
PYR test – positive
Ø Serological test:
Anti streptolysin o (ASO) is most widely used
Ø Antigen detection test:
ELISA
Agglutination test
Ø Molecular method:
Polymerase chain reaction
Ø Antibiotic susceptibility testing:
Oral penicillin V or amoxicillin
B. GRAM POSITIVE BACILLIRAM POSITIVE COCCI .
BACILUS ANTHRAX
# Morphology
· Gram positive bacilli
· Non-acid-fast
· Non-motile
· Size: 3- 10 µm
· Shape: rod shaped
· Spore forming bacillus
# Pathogenesis
Ø Source of infection – Contaminated food & water, contaminated animal product, air droplet.
Ø Mode of transmission – transmitted by direct or indirect content, ingestion & inhalation.
Ø Route of transmission – respiratory tract, GI tract, etc.
Ø Incubation period – about 1 to 7 days.
· Anthrax is primarily a disease of animal like cattle & sheep, less often of horse & swine.
· Direct spread of disease from animal to animal is rare.
· Anthrax is usually septicemia but may sometimes be localized.
HUMAN ANTHRAX:
· Human are occasionally secondary infected from disease animal.
· There are three clinical type of infection based on route of infection.
1. Cutaneous infection:
Entry of spore through the skin.
Face, neck, hand & back are commonly affected site.
Commonly seen in farmer or person handling carcasses.
2. Pulmonary infection:
Pulmonary anthrax is due to inhalation of the dust or filament of wool from infected animal, particular seen in wool facories.
Also called wool sorter’s disease.
3. Intestinal infection:
It is rare & seen in person who take improper cooked infected meat.
# Lab diagnosis
Ø Specimen:
Throat swab
Fluid
Pus
Sputum
Blood
Ø collection & transport:
Specimen should be collected on sterile container.
Ø Microscopy:
Gram staining - Gram positive bacilli seen.
Ø Culture:
Best grow in nutrient agar at 37®C for 24-48 hours.
Ø Colony morphology:
After growth medusa head appearance colonies appear.
Ø Molecular method:
Polymerase chain reaction
Ø Antibiotic susceptibility testing:
Ciprofloxacin
Doxycycline
GRAM NEGATIVE BACTERIA
C. GRAM NEGATIVE COCCIGRAM NEGATIVE COCCI .
NEISSERIA MENINGITIDIS
# Morphology
· Gram negative cocci
· Shape: spherical or oval cocci
· Size:0.6- 0.8 µm in size
· Motility: non-motile
· Flagella: non-flagellated
· Spore: non-sporing
· Arrangement: in pairs (diplococcic)
# Pathogenesis
Ø Source of infection – droplets of respiratory secretions.
Ø Mode of transmission – transmitted by kissing, sneezing or coughing.
Ø Route of transmission – respiratory tract
Ø Incubation period – about 3 to 4 days.
· N. meningitidis causes pyogenic meningitis in all ages.
· Meningococci are strict human pathogens, Common in children and young adults.
· The other bacterial agents responsible for pyogenic meningitis include H. influenzae and Str. pneumoniae.
· The organism may spread along the perineural sheath of the olfactory nerve, through the cribriform plate to the subarachnoid space or through the blood stream.
# Lab diagnosis
Ø Specimen:
CSF
Blood
Nasopharyngeal swab
Ø collection & transport:
Specimen should be collected on sterile container.
Lumbar puncture for CSF & vein puncture for blood.
Ø Microscopy:
Gram staining - Gram negative diplococci seen.
Ø Culture:
Inoculated on blood agar or chocolate agar.
The plate is incubated at 35-36°C under 5- 10% CO2.
Colonies appear after 18- 24 hours.
Ø Colony morphology:
In solid media colonies appear
Shape – round
Size - 1mm
Surface – convex
Color – grey
Opacity – translucent
Ø Biochemical reaction:
Catalase test – positive
Oxidase test – negative
Ø Molecular method:
Polymerase chain reaction
Ø Slide Agglutination
Direct slide agglutination of the organism may be done with specific antisera.
Ø Antibiotic susceptibility testing:
penicillin
D.GRAM NEGATIVE BACILLI
ESCHRICHIA COLI (E.COLI)
# Morphology
· Gram negative bacilli
· Shape: rod shapes bacteria
· Size: 1- 2 µm in size
· Motility: some strain of bacteria are motile
· Flagella: some bacteria are motile
· Spore: non-sporing
# Pathogenesis
Ø Source of infection – contaminated food and water
Ø Mode of transmission – transmitted direct contact with infected person and animal
Ø Route of transmission – ingestion, inhalation, etc.
Ø Incubation period – about 2 to 4 days.
· There are four major types of clinical syndromes which are caused by Esch. coli:
1. Urinary tract infection
2. Diarrhoea
3. Pyogenic infections
4. Septicaemia
# Lab diagnosis
Ø Specimen:
Midstream urine
Ø collection & transport:
Specimen should be collected on sterile container.
Send it to the laboratory with minimum delay.
Ø Microscopy:
Gram negative bacilli seen
Ø Culture:
Inoculated on mac-conkey agar
The plate is incubated at 37°C for 24-48 hours
Colonies appear after 18- 24 hours.
Ø Colony morphology:
In solid media colonies appear
Shape – circular
Size – 2-3mm
Surface – smooth
Edge – entire
Color – pink due to lactose fermentation
Opacity – opaque
Ø Biochemical reaction:
Catalase test – positive
Oxidase test – negative
Indole test – positive
Methyl red – positive
VP – negative
Citrate - negative
Ø Molecular method:
Polymerase chain reaction
Ø Antibiotic susceptibility testing:
Antimicrobial susceptibility testing can be performed to determine the most effective antibiotics for treating the infection.
RECENT ARTICLE
Autoclave: https://www.docnotemaster.in/autoclave
Muscular system: https://www.docnotemaster.in/muscular-system
Torch profile: https://www.docnotemaster.in/torch-profile-test
Rheumatoid arthritis: https://www.docnotemaster.in/rheumatoid-arthritis-ra
Introduction of anatomy: https://www.docnotemaster.in/introduction-of-anatomy
Morphology and physiology of bacteria: https://www.docnotemaster.in/morphology-and-physiology-of-bacteria