online learning with Doc note master|| Himanshu paneru
STERILIZATION AND DISINFECTION
The aim of sterilization and disinfectant is to control the spread of harmful microorganisms such as bacteria, viruses, and fungi, that can cause infections and harmful for human health.
GENERAL MICROBIOLOGY
Himanshu Paneru
4/14/20247 मिनट पढ़ें


STERILIZATION AND DISINFECTION
Sterilization and disinfection are essential processes that maintain health and safety across various industries including healthcare, food production, and public health.
The aim of sterilization and disinfectant is to control the spread of harmful microorganisms such as bacteria, viruses, and fungi, that can cause infections and harmful for human health.
STERILIZATION
Sterilization is defined as a process by which an article, surface, or medium is free of all living microorganisms including bacteria, viruses, fungi, and their spores, as well as other microorganisms either in the vegetative or in the spore state.
DISINFECTANT
Disinfection refers to the use of a chemical agent that destroys or removes all pathogenic organisms or organisms capable of giving rise to infection. This process destroys vegetative pathogens but not bacterial endospores.
Disinfection is the process of reducing the number of pathogenic microorganisms. All organisms may not be killed but the number is reduced to a level that is no longer harmful to health.
ANTISEPTIC
An antiseptic is a substance or agent that inhibits the growth of active microorganisms, which can safely be applied to living tissues and are used to prevent infection by inhibiting the growth of microorganisms.
PRINCIPLE OF STERILIZATION AND DISINFECTANT
STERILIZATION: It is the process of completely destroy all forms of microorganism and spores. It is essential for absolute sterility in medical and laboratory environments where any microbial contamination can be hazardous.
Sterilization method include autoclaving, hot air oven, radiation, filtration.
DISINFECTANT: It reduces pathogenic microorganisms to level which is safe for health making it suitable for non-critical surfaces and environments.
Common disinfection methods include chemical disinfectants (alcohol, aldehyde, phenols, dyes) and physical methods such as pasteurization and UV radiation.
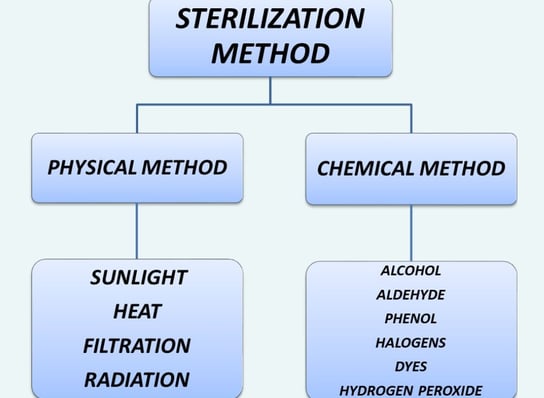
METHODS OF STERILIZATION
PHYSICAL METHOD
1. Sunlight:
· Sunlight has an active germicidal effect due to its content ultraviolet ray (UV). It is a natural method of sterilization for water in tanks, rivers and lakes.
2. Moist heat sterilization:
a. Sterilization at a temperature 100°C
Pasteurization -
· Two methods of pasteurization are followed:
· Flash method and holder method.
In the flash method, milk is exposed to heat at 72°C for 15–20 seconds followed by a sudden cooling to 13°C or lower.
In the holder method, milk is exposed to a temperature of 63°C for 30 minutes followed by cooling to 13°C or lower, but not less than 6°C.
Vaccine bath –
· Bacterial vaccines are sterilised in special vaccine baths at 60°C for one hour.
b. Sterilization at a temperature of 100°C
Boiling –
· Boiling of water for 10–30 minutes kills most of the vegetative forms of bacteria but not bacterial spores.
· This method is not recommended for sterilization surgical instrument.
c. Sterilization at a temperature 100°C
Autoclave: https://www.docnotemaster.in/autoclave
Tyndallization:
· It is a method of sterilization that involves intermittent heating of a substance over several days to destroy heat-resistant spores and other microorganisms.
3. Dry heat sterilization:
a. Flaming: Glass slides, scalpels, and mouths of culture tubes are sterilized by passing them through the Bunsen flame without allowing them to become red hot.
b. Incineration: Incineration is a method of sterilization that involves the complete destruction of microorganisms and other organic materials by exposing them to high temperatures.
c. Hot air oven:
· Most common method of sterilization by dry heat.
· Hot-air oven is used in laboratories and clinics for heat resistant items that are not sterilized well by moist heat.
· The oven is electrically heated and is fitted with a fan to ensure adequate and even distribution of hot air in the chamber.
· It is also fitted with a thermostat that ensures circulation of hot air of desired temperature in the chamber.
Principle
· Dry heat sterilization denatures proteins and oxidizes cellular components, leading to the destruction of microbes.
Temperature and time
· 160° for 2 hours is required for sterilization
· Other - alternative temperatures
· 170°C for one hour and
· 180°C for 30 minutes.
Uses
· Glasswares (syringes, Petri dishes, flasks, pipettes, test tubes, etc.).
· Surgical instruments (scalpels, scissors, forceps, etc.).
· Chemicals (liquid paraffin, sulfonamide powders, etc.).
2. Filtration:
· This method of sterilisation is useful for substances which get damaged by heat process e.g. sera, sugars, antibiotic solutions.
· Commonly used for sterilizing air, water, and heat-sensitive liquids such as culture media and pharmaceuticals.
3. Radiation:
· The ionizing and nonionizing radiations are the two types of radiation used for sterilization.
· Gamma radiation from a cobalt-60 source is used for sterilization of antibiotics, hormones, sutures, catheters, animal feeds, metal foils, and plastic disposables such as syringes. This has also been used to sterilize and ‘pasteurize’ meat and other food items.
CHEMICAL METHOD
· Several chemical agents are used as antiseptics as well as disinfectants.
· DISINFECTANT: Disinfectants are chemical agents which reduce the number of microorganisms which is no longer harmful.
· ANTISEPTICS: Antiseptic are chemical agent which is safely use on living tissue.
PROPERTIES OF DISINFECTANT AND ANTISEPTIC
· An ideal antiseptic or disinfectant should possess several key characteristics to be effective, safe, and practical for use.
It should be effective against microorganisms, including bacteria, viruses, fungi, and spores.
Act quickly to kill or inhibit the growth of microorganisms.
Be stable and effective in acidic as well as in alkaline condition
It should be safe to use
Compatible with other disinfectant
Cheap and easily Available
Have minimal impact on the environment and be biodegradable when possible.
Not cause local irritation
Factor affecting action of disinfectant
· Type of Microorganism:
o Different types of microorganisms (bacteria, viruses, fungi, spores) have different levels of resistance against disinfectants.
· Concentration:
o The concentration of the disinfectant affects its impact. Higher concentrations are often more effective, but it will used as guidline.
· Contact Time:
o Disinfectants need sufficient contact time with the surface or object to effectively eliminate microorganisms.
· Temperature:
o Increase in temperature increases the efficiency of disinfectants.
· pH Level:
o The pH level of the disinfectant and the environment can impact its effectiveness. Disinfectants may work best at specific pH levels.
· Storage and Shelf Life:
o Proper storage conditions and adherence to the product's shelf life are essential for maintaining disinfectant potency.
· Compatibility;
o The disinfectant should be compatible with the surfaces and materials it is used on.
· Safety and Toxicity:
o Disinfectants must be safe for use, with minimal risk of toxicity or harm to humans, animals, and the environment.
Types of chemical disinfectant
1. Alcohols:
· They act by denaturing bacterial proteins.
· Common Types: Ethanol and isopropanol.
· Effectiveness: Effective against a wide range of microorganisms, including bacteria and some viruses.
· Use: Commonly used as skin antiseptic, used at a concentration of 60-70 % in water
2. Chlorine Compounds:
· Common Types: Bleach (sodium hypochlorite) and chlorine dioxide.
· Effectiveness: Highly effective against bacteria, viruses, and fungi.
· Use: Often used for disinfecting water supplies, swimming pools, and surfaces.
3. Aldehydes:
· Common Types: Glutaraldehyde and formaldehyde.
· Effectiveness: Highly effective against bacteria, viruses, fungi, and spores.
· Use:
Preservation of tissue for histological examination.
Sterilise bacterial vaccines.
For killing of bacterial cultures and suspensions.
For destroying anthrax spores in hair and wool
4. Phenol:
· Common Types: Phenol and o-phenylphenol
· Effectiveness: Effective against bacteria and fungi, with limited activity against viruses.
· Use: Used for disinfecting surfaces in healthcare
5. Hydrogen Peroxide (H2O2):
· Effectiveness: Effective against bacteria, viruses, and fungi.
· Use: Used for surface disinfection, medical instrument cleaning, and wound care.
6. Halogens:
· Chlorine and iodine are two commonly used disinfectants. These are bactericidal and are effective against sporing bacteria and viruses.
7. Dyes:
· The dyes that have been used extensively as skin and wound antiseptics include
(a) acridine dyes
(b) aniline dyes.
Use of sterilization and disinfectant
Sterilization
· Surgical instruments and medical devices
· Laboratory equipment and Glassware (syringes, Petri dishes, flasks, pipettes, test tubes, etc.).
· Sterilization of drugs and other pharmaceutical products
· In food industry for packaging
Disinfectant
· Used on medical equipment, hospital rooms, and patient care areas to reduce the risk of infection.
· used for hand hygiene and skin antisepsis
· Disinfection is important in water treatment
Recant article
Autoclave: https://www.docnotemaster.in/autoclave
Muscular system: https://www.docnotemaster.in/muscular-system
Torch profile: https://www.docnotemaster.in/torch-profile-test
Rheumatoid arthritis: https://www.docnotemaster.in/rheumatoid-arthritis-ra
Introduction of anatomy: https://www.docnotemaster.in/introduction-of-anatomy
Morphology and physiology of bacteria: https://www.docnotemaster.in/morphology-and-physiology-of-bacteria